When Time Became the Last Treatment: A Father, a Hospital Room, and the Cost of Being Certain Too Soon

He pulled a gun in a hospital room.
Not to hurt anyone.
Not out of rage.
But to stop a goodbye that felt too final.
It was 2015, inside a hospital in Houston. Doctors had delivered the words no parent ever wants to hear: there was no hope. The son had suffered a massive stroke. Life support would be withdrawn. The process would be clinical, legal, and irreversible.
A terminal wean.
To medicine, it was the next step.
To a father, it was the end of everything.
When medicine reaches a conclusion — and love does not
Hospitals are built on protocols. On evidence. On experience earned through thousands of cases. Doctors are trained to recognize when recovery is no longer possible, and to prevent prolonged suffering when the outcome is believed to be certain.
But certainty is a dangerous word.
Because for families, certainty does not feel scientific — it feels absolute.
In that room, the father did not see charts or prognosis. He saw his child. He saw a body still warm, a chest still rising with mechanical breath, a life that felt unfinished.
And he panicked.
A moment that froze an entire floor
The father locked himself inside the hospital room.
He had a gun.
Police surrounded the floor.
For hours, the hospital stood still.
No shots were fired.
No one was harmed.
This was not about anger. It was about time.
A father watching the clock run out on his child — and refusing to let the hands keep moving.

A small response that changed everything
During the standoff, the father made a request.
Ask my son to squeeze my hand.
And according to those present, the son did.
It was not dramatic.
It was not proof of recovery.
But it was enough to raise doubt.
Enough to pause the withdrawal of life support.
Enough to slow a process that had already been set in motion.
Sometimes, in medicine, doubt is powerful.
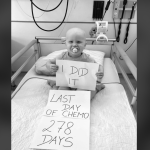
What happened next
Eventually, the father surrendered peacefully.
The situation ended without violence.
And the son?
He lived.
Over time, he regained consciousness.
Later, he spoke publicly about his recovery.
That part is real. Documented by major U.S. news outlets.
This was not rumor.
It was not exaggeration.
But it was also not a miracle that rewrote science.
The uncomfortable truth behind the story
True brain death, as defined by medicine, is irreversible. It is not a coma. It is not a severe brain injury. It is death.
Many doctors later said that the diagnosis in this case may not have met that standard.
That distinction matters.
This story is not evidence that brain death can be reversed.
It is evidence that certainty must be used carefully.
Because when decisions involve life and death, being wrong too soon can be just as devastating as being wrong too late.
What this story is — and what it is not
This story is not an argument for guns in hospitals.
They do not belong there.
It is not a justification for threats or force.
Those actions were dangerous and unacceptable.
But it is a story about how fragile end-of-life decisions become when time, fear, and love collide.
It is a story about:
-
How parents experience medical finality
-
How panic can override reason
-
How systems must balance authority with humility
And how sometimes, the most dangerous thing in the room is not a weapon — but certainty that leaves no room for pause.
The role of time in healing
Medicine saves lives every day.
Protocols protect patients.
Expertise matters.
But time itself can also be a form of treatment.
Time allows swelling to decrease.
Time allows the brain to surprise us.
Time allows uncertainty to reveal itself.
In this case, time made the difference.

Why this story still matters
Years later, this story continues to circulate — not because of the gun, but because of the question it raises:
How sure is sure enough?
For families facing end-of-life decisions, this story highlights the need for:
-
Clear communication
-
Compassionate explanation
-
Space for second opinions
-
And respect for the emotional reality of loss
For medical professionals, it reinforces the importance of humility — even when experience suggests an outcome is unlikely.
A warning, not a model
This should never be a template.
No family should feel that force is the only way to be heard.
No hospital should ever be placed in such danger.
But it should serve as a warning.
A warning about rushing finality.
A warning about failing to acknowledge uncertainty.
A warning about how fear and love can push people beyond reason when time disappears.
In the end
This was not a story about defiance.
It was a story about desperation.
Not about rejecting medicine — but about begging for one more chance to believe in life.
Sometimes, the hardest decisions demand not just expertise, but patience.
Because in rare moments, being wrong too soon costs more than waiting ever could.